IdeaLab: A Smart Clinic Empowered by Data
Every IdeaLab charrette starts with a 'fill the wall' exercise, where teams share their research, initial thinking and concepts.
SmithGroup's IdeaLab is a research and innovation process that gives us the creative space—outside of everyday project concerns—to study future healthcare and other industry disruptors in depth. As part of this initiative, we explore the inventions, products, technologies, and strategies that are in the pipeline (or not yet imagined) to anticipate what these will mean for the industry and, most importantly, for our clients.
Our first IdeaLab exploration is focused on Artificial Intelligence (AI). Industry experts and three teams of SmithGroup health professionals convened to imagine what true potential lies within AI and how it could disrupt the healthcare industry—both for better and for worse—today, tomorrow and decades down the road. The IdeaLab teams were presented with this challenge: can you design a clinic, for the year 2035, that is run entirely by an artificial intelligence, with little or no human-to-human interaction?
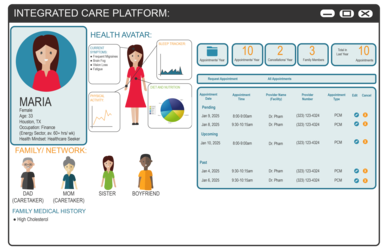
In our scenario, in the year 2025 artificial intelligence and technology have made tremendous advancements throughout the healthcare sector. Each team was given a user persona/patient to guide our future thinking: our patient is Maria, and her world is more intelligent than ever, responding to her needs and gathering information from nearly every aspect of her life through wearables and other digital devices. To provide a comparative understanding of Maria’s health, massive amounts of patient data can be aggregated and compared using machine learning systems to define an ever more exact understanding of disease etiologies and treatments. But, while Maria’s world is rapidly becoming more digitally connected, human beings are becoming more socially disconnected. In the coming age of AI, there will be a need for a new type of integrated care platform, which we call ICP2025.
Telemedicine through her home computer is Maria’s first point of contact with her primary care physician. Her wearables have been keeping track of her sleep patterns so that her physician can already access that information.
In 2025, driverless cars, automated systems, and self-serve kiosks reduce the need for daily human interaction—a trend that, while useful in saving time and removing friction from routine activities, creates a lonelier, more isolated world.
Maria’s healthcare provider recognizes the benefits that these new technological advancements offer for affordability and quality of healthcare, but she is also sensitive to the issues that can arise with fewer human interactions. The result is that, by the year 2025, Maria’s primary care physician (PP) plays a significantly greater role in the diagnosis and treatment of many of her symptoms with the help of technology.
Maria’s primary physician is the heart of her medical team, but the Integrated Care Platform (ICP2025) is its nerve center. Maria’s complex set of symptoms points to no well-known and discrete diagnosis, so a wide array of data and knowledge needs to be applied to her case.
In the present-state system of care, Maria’s physician applies her knowledge, augmented by discrete tests, database searches, and expert consultation to determine a diagnosis and treatment. This system is slow, ad hoc, divided by institutional and geographic boundaries, and dependent upon human motivation. It is prone to confusion, missed connections, and often leads to dead ends.
In 2025, Maria’s primary physician is the human, social connection to this rather confusing world of medical knowledge, assisted by AI. The primary is empowered by a new generation of small diagnostic equipment, a shift that moves most non-invasive diagnostic testing procedures into the PP clinic setting. The PP is also freed from many of the tasks that reduce her availability to work with patients: including billing, form-filling, arranging consults, and medical record upkeep.
Aiding human interaction through increased speed to treatment and diagnosis will be the biggest advantage of AI. If machines are able to take away some of the data research and simple repetitive tasks of a typical care visit, humans will be able to concentrate on the compassion and reasoning that machines will never be able to replicate.
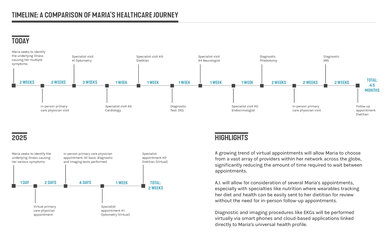
Maria's Touchpoints: Telemedicine through her home computer is Maria’s first point of contact with her primary care physician. Her wearables have been keeping track of her sleep patterns so that her physician can already access that information. Through the AI care assessment an appointment is made and Maria will meet her physician in a few days. The office setting has a care room that is connected to a suite of diagnostic imaging equipment. Maria’s appointment is quick and efficient. She spends half an hour relaxing while her records are run through the Integrated Care Platform. Her diagnosis is explained to her on an interactive smart board, and her treatment plan is well in hand before she leaves the building.

"Primary Care Plus" design concept: Incorporation of nature into the primary care environment is a key design driver. A green wall situated behind the welcome desk greets patients upon arrival. Several rooms within the suite look out into a lush outdoor garden space which also serves as a waiting area for patients and their guests.

Some of our early research led us to questions about the reliability of artificial intelligence. Left unchecked, would humans be left out of the care equation? We couldn’t believe that human reasoning and human touch did not have a place in tomorrow’s healthcare environment. Would robots be replacing humans?
But the exciting possibilities of machine learning to improve the diagnosis and treatment of complex problems began to energize our project. Envisioning the future was all about imagining how technology could benefit the care environment while empowering human connection. As an aid to human interaction, computers can speed up data and research searches, scan and transfer records, and take over the repetitive tasks of the healthcare practice. In the competitive, value-added, cost-cutting world of healthcare, being lean means having machines do what work they can and freeing caregivers to provide the reasoning and compassion that machines cannot.
Learn more about IdeaLab or the other IdeaLab teams' findings, The Driverless Clinic, and Better Access through AI. Download our full report here.